Immune Cell Enzyme Links the Body and Brain During Stress
Levels of a specific immune cell enzyme are increased in stressed mice and in patients with major depressive disorder.
Complete the form below to unlock access to ALL audio articles.
Chronic stress a risk factor for neuropsychiatric disorders
We all experience stress to some degree – it’s a natural part of the human experience. Stress – in small doses – can even be beneficial; it might serve as motivation for us to address challenges that we are facing or make changes in our lives.
Chronic stress, however, can have detrimental effects on our wellbeing and is considered a primary risk factor for a number of neuropsychiatric disorders, including major depressive disorder (MDD). Understanding how stress contributes to the pathophysiology of such disorders is a pertinent research area.
What is major depressive disorder?
Depression is described as an experience of low mood that persists. It can range in seriousness from mild, temporary episodes to severe, more persistent depression. Clinical depression is the most severe form and is also referred to as MDD. MDD might be diagnosed if an individual persistently presents with symptoms including low or depressed moods, anhedonia – a lack of interest or pleasure from life experiences – feelings of guilt or low worth, low energy, issues with concentration, changes in appetite, sleep disturbances or suicidal thoughts.
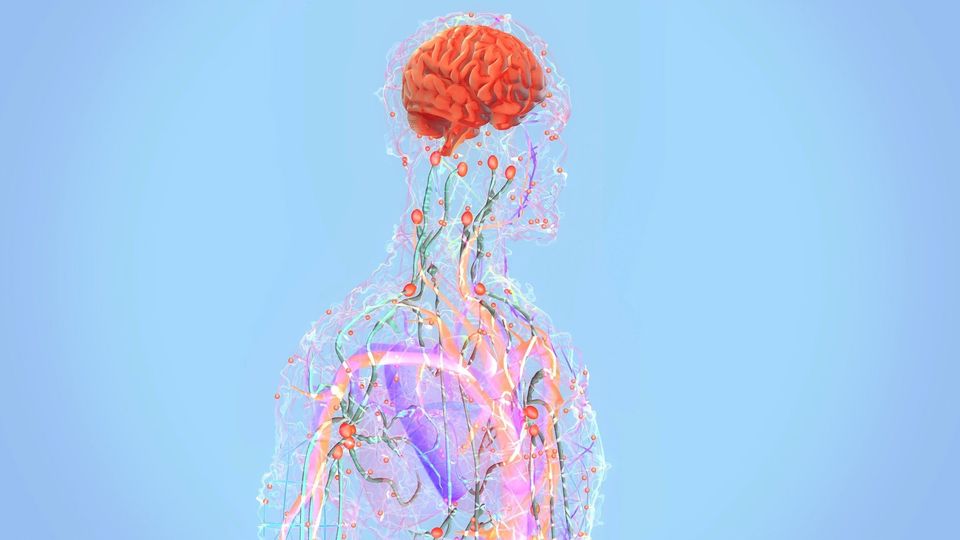
Stress can affect how the central nervous system (CNS) – the brain and the spinal cord – interacts with physiological processes occurring in the rest of the body, such as the immune system.
Studies of blood samples taken from patients with MDD show increased circulation of pro-inflammatory cytokines, among other immune cells, indicating low-grade inflammation. In mice, stress can disrupt the blood–brain barrier, permitting circulating proteins, such as those produced by the immune system, direct entry into the brain. While much research has linked disturbances in the peripheral immune system with stress-related disorders, the biological mechanisms that underpin this link are not yet understood.
A collaboration of scientists, including teams from the University of Zurich, the University Hospital of Psychiatry Zurich (PUK) and the Icahn School of Medicine at Mount Sinai, provide new evidence that a specific enzyme found in immune cells could be that link. The research, which according to the authors indicates a “new body–mind mechanism”, is published in Nature.
Matrix metalloproteinases play an important role in maintaining ECM homeostasis
Neurons and other cells are separated by extracellular spaces that contain interstitial fluid and the extracellular matrix (ECM), which plays a significant role in regulating synaptic plasticity and function. The ECM is broken down and rebuilt by a number of different enzymes, including enzymes called matrix metalloproteinases (MMPs).
MMPs also regulate functions related to inflammation and have been associated with inflammatory disorders such as cancer and heart attacks. Currently, we don’t know all that much about how MMPs produced in the periphery might affect the brain in the context of stress.
In the new study, the research team explored the effects of stress on the immune system and the brain of mice, which revealed novel insights into the role of MMPs.
Increased MMP-8 expression in stress-susceptible mice and humans with MDD
The study utilized the chronic social defeat stress (CSDS) paradigm, which is considered to be one of the most suitable mouse models of psychosocial stress. It is commonly used to test the efficacy of antidepressant therapy candidates.
The CSDS paradigm involves subjecting a mouse to subordination by another, aggressive mouse, through physical contact and sensory exposure over a period of 10 days. In response, some mice exhibit behaviors that mimic stress in humans, such as social avoidance, reduced preference for rewards and impaired social rewards. On the physiological level, they present with metabolic syndromes, inflammation and gastrointestinal issues. These mice are referred to as stress-susceptible (SUS) mice.
A portion of mice subjected to the CSDS paradigm do not exhibit such responses; rather, their behavioral and physiological profiles more closely reflect unstressed control (CON) mice, and so they are referred to as resilient, or RES, mice.
The researchers, led by Dr. Flurin Cathomas, a psychiatrist and neuroscientist at the University of Zurich, conducted immune cell profiling, RNA-sequencing and whole-brain analyses across SUS, CON and RES mice.
In SUS mice, the CSDS paradigm increased the migration of monocytes – a type of leukocyte – to the vascular system of the brain. “Both circulating monocytes and monocytes that traffic to the brain showed increased MMP-8 expression following CSDS,” the researchers described.
MMP-8 directly infiltrated the nucleus accumbens, part of the brain’s reward system, where it was associated with neurophysiological and behavioral changes. “If MMP-8 penetrates the brain tissue from the blood, it changes the matrix structure and thus disrupts the functioning of the neurons. Mice who are affected by this process display changes in behavior that are similar to those seen in humans with depression,” said Cathomas.
By knocking out the gene encoding MMP-8, the team could investigate whether it was responsible for the behavioral changes observed. Sure enough, compared to control mice, MMP-8 knock-out animals did not exhibit stress-related behavioral changes.
Cathomas and colleagues explored whether stress caused similar immune profile changes in humans by analyzing blood samples from 29 healthy individuals and 40 individuals with MDD. “Blood analyses of patients with depression indicate that the findings from the mouse models are also relevant for humans: both the monocytes and MMP-8 were increased in the blood of people with depression in comparison to healthy participants,” Cathomas explained.
A new body–mind mechanism?
The data highlight a mechanism by which peripheral immune molecules can directly affect the CNS in the context of social stress. “They [the findings] indicate a new ‘body–mind mechanism’, which might be relevant not only for stress-related mental illness, but also for other diseases that affect both the immune and nervous systems,” said Cathomas.
He added that the role identified for MMP-8 in this mechanism could open doors for novel therapeutics targeting depression. “Targeting specific peripheral immune cell-derived matrix metalloproteinases could constitute novel therapeutic targets for stress-related neuropsychiatric disorders,” the authors conclude, though further research exploring the mechanism in humans will be necessary.
Reference: Cathomas F, Lin HY, Chan KL, et al. Circulating myeloid-derived MMP8 in stress susceptibility and depression. Nature. 2024. doi:10.1038/s41586-023-07015-2