There’s More to the Vagus Nerve Than “Rest and Digest”
Limiting the vagus nerve to “rest and digest” could overlook its involvement in broader physiological processes.

Complete the form below to unlock access to ALL audio articles.
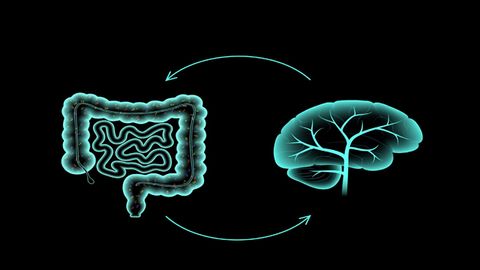
The vagus nerve, nicknamed the “wandering” nerve due to its widespread distribution throughout the body, plays a pivotal role in our internal communication system. By relaying sensory information from a variety of peripheral organs and tissues to the central nervous system (CNS), it is integral to a wide range of brain–body processes.
Vagal activity has been associated with the body’s “rest and digest” functions – those orchestrated by the autonomic nervous system (ANS) that typically have an inhibitory or “slowing” effect. However, research is beginning to question this idea, suggesting that by limiting the function of the vagus nerve to merely “rest and digest”, we may be overlooking its involvement in broader physiological processes and even behaviors.
In 2022, Technology Networks interviewed Professor Nils Kroemer, a researcher in the neuroMADLAB at the University Hospitals of Tübingen, Bonn and University Hospital Bonn, whose work centers around the neurobiological principles of desire, motivation and action.
Kroemer and colleagues had published a paper in Brain Stimulation showing – for the very first time – that non-invasive vagus nerve stimulation (VNS) could strengthen communication between the gut and the brain within a few minutes. The researchers also found that this coupling effect spread across regions of the brain that are associated with higher-order cognitive functions, including goal-directed behavior.
In Trends and Cognitive Science, Kroemer now outlines a theory that the vagal afferent pathway helps to support transitions between different survival modes, and regulates reward signaling.
Written with Dr. Vanessa Teckentrup – a former PhD student in Kroemer’s lab, now a researcher in the Gillan Lab at Trinity College Dublin – the review proposes that this theory could help us to understand links between bodily symptoms and motivation.
We sat down with Kroemer to discuss the theory and what it might mean for our understanding of nervous system disorders.
Molly Campbell (MC): For many years, the function of the vagus nerve has been associated with the “rest and digest” aspect of the human nervous system. Why is this?
Nils Kroemer (NK): The vagus nerve is part of parasympathetic nervous system (PNS). Stimulating the vagus nerve releases acetylcholine, the primary neurotransmitter of the PNS. It is thought to be predominate in quiet “rest and digest” conditions while the sympathetic nervous system (SNS) drives responses to stressful situations – think “fight or flight”.
Hence, it is assumed that the main purpose of the PNS is to conserve energy to be used later and to regulate bodily functions, such as digestion and heart rate, to facilitate recovery.
What are afferent and efferent nerves?
Afferent nerves deliver information from sensory receptors to the brain.
Efferent nerves transport signals from the brain to the periphery, initiating a physiological response.
MC: What are some of the key studies that demonstrate the vagus nerve has a role in broader functions, including goal-directed behavior?
NK: The most conclusive evidence comes from studies in rodents using highly controlled experiments with invasive stimulation techniques.
For example, a seminar paper by Ivan de Araujo’s lab published in Cell in 2018 showed that stimulation of the right nodose ganglion leads to dopamine release in the brain, and conditions preferences for flavors and places. Moreover, the stimulation is inherently rewarding, since animals will work to self-stimulate their brain through vagal afferent projections.
The nodose ganglia
The nodose ganglia are a pair of structures within the autonomic nervous system. Part of the vagus nerve, they receive input from the sensory neurons located in organs such as the heart, lungs and digestive organs.
Additional studies in animals have shown that stimulating vagal afferents affects prospective reward seeking. This is a hallmark of goal-directed behavior, since simple homeostatic behavior is reactive and triggered only once an energy deficit is experienced.
In humans, we have successfully translated these findings by showing enhanced invigoration of effort for rewards during right-sided VNS. These results were published in Nature Communications in 2020.
Since then, we and others have reported various additional effects of VNS that are difficult to reconcile with a narrow role of vagal afferents in facilitating rest and digest. For example, several studies have reported that vagus nerve stimulation reduces the frequency of gastric myoelectric activity, a marker of the digestive speed of the gastrointestinal tract. In other words, this would slow rather than facilitate the digestion of food.
MC: Your review paper proposes a unifying framework, which integrates vagal functions in sensing bodily states with state-dependent tuning of reward sensitivity and instrumental actions. This means that organisms can effectively switch between the survival modes of “rest and digest” to “strive and survive”. Can you explain this framework?
NK: The idea is simple and straightforward in its core.
Our organ systems function best if they are constantly kept within a limited range that we call homeostasis. If we take the gastrointestinal tract as an example, it relies on the brain to direct behavior towards food if energy stores of the body are depleted, to keep it in balance.
We now propose that vagal afferents play a crucial role in deciding whether we should pay attention to the ascending signals from the body. If vagal afferents are stimulated, the brain will assign a greater weight to signals of the body, allowing us to focus more on the intrinsic needs of the body. Arguably, those needs go well beyond rest and digest and include prospective reward-seeking, so that we make sure to always have enough food to keep the body running.
In our opinion, this simple idea may explain a wide range of observations and ultimately help us understand prominent links between bodily symptoms, such as fatigue, and motivational as well as affective consequences.
MC: If vagal functions are central to organisms being able to switch effectively from “rest and digest” to “strive and survive”, what implications might this have for our understanding of the nervous system, and disorders of the nervous system?
NK: We believe that it might be worth taking a second look at several disorders that we currently refer to as “mental” disorders.
For example, somatic symptoms of depression might be better understood by disturbances in brain–body interactions. There is also growing evidence for a mechanistic role of such disturbances in anxiety and stress-related disorders, but eating and metabolic disorders are plausible candidates as well.
A dysregulation between signals originating from peripheral organ systems, such as the gut, and the brain might contribute to mood disturbances and changes in motivation that have been difficult to understand and treat by looking at the brain alone.
MC: Can you explain what VNS is, how it is being used and how your perspective on how vagal afferent signaling in humans might help to clarify the results observed in VNS studies?
NK: VNS typically uses electrodes to administer a current that triggers a signaling cascade in the target regions of the nerve in the brain.
This stimulation is intended to emulate the endogenous activation of the nerve, for example, as achieved by nutrient sensing in the gastrointestinal tract. Invasive VNS has been used for more than three decades now. Initially developed as an adjunct treatment for epilepsy, anti-depressive effects of the stimulation were observed in patients with epilepsy, who did not even show improvements in their neurological symptoms.
Non-invasive VNS was then developed as a scalable alternative that could be used at an earlier stage of a disorder. It has shown comparable effectiveness in the treatment of various conditions, but large head-to-head comparisons with invasive VNS are still lacking.
Nevertheless, non-invasive vagus nerve stimulation provides a great opportunity to study the role of vagal afferent signals in healthy humans as well. Ultimately, this may help us understand the vital role of vagal afferents in the control of human behavior, which could pave new ways for improved behavioral interventions.
MC: What effect do you hope the publication of this review will have? Are there any particular studies that you would like to see being conducted?
NK: We are still at an early stage of research, specifically in humans. For example, the conventional stimulation protocols have not been optimized for specific indications yet. Do we just need to make sure that we are effectively stimulating the vagus nerve, or are some treatment regimens better for motivational symptoms compared to peripheral inflammation?
I feel very passionate about the necessity to understand how acute effects of VNS translate to long-term benefits in behavior and heath. To this end, we need larger studies, with thorough designs, to get to the bottom of some of the pressing issues to increase the chances for an effective treatment in the long run.
MC: Is there anything further that you would like to share with our readers on this topic?
NK: We hear from many patients who are suffering from various somatic symptoms and hope that VNS will help improve their condition soon. We are also eager to quickly provide better treatments with minimal side-effects, but it will likely take a few more years before they become more widely accessible after thorough investigations and clinical monitoring.
In the meantime, there are many clinical studies now running to evaluate the effectiveness of non-invasive vagus nerve stimulation for various conditions. There might be options to support this important and promising research.
Professor Nils Kroemer was speaking to Molly Campbell, Senior Science Writer for Technology Networks.